On the morning of September 21, 1993, a shy and intelligent American woman who had never practiced Buddhism took an elevator to an upper floor of Duke Medical Center in Durham, North Carolina. Her name was Susan Kandel, and she was 37. Panicked and miserable because her trusted therapist had recently moved to another state, she walked onto an open breezeway and jumped, expecting to fall ninety feet to her death. She landed instead on a maintenance workers’ platform forty feet below and was taken to the emergency room with three broken vertebrae. A month later, wearing a body brace but not paralyzed, she was involuntarily committed to John Umstead state psychiatric hospital, an aging brick building on the outskirts of Durham, N.C. She, the hospital staff and her family all expected her to be there for a long, long, time, and she was in deep despair.
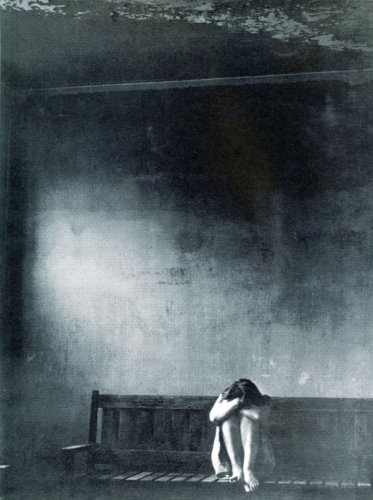
It was her fourth commitment to John Umstead hospital and her seventh serious suicide attempt. She had been given the damning psychiatric diagnosis of Borderline Personality Disorder as a teenager and had spent much of her life turning on a wheel of suffering from suicide attempt to mental hospital to halfway house to suicide attempt. Much like a distressed monkey gnawing its knuckles in a small cage at the zoo, she had discovered at 17 that cutting her forearms with razor blades made her feel somewhat better. At 19, she was sent to a mental hospital for the first time and there she first tried to kill herself.
Nearly two decades passed and therapy fashions changed, but nothing made any appreciable difference—not shock treatment, talk therapy, or psychiatric drugs; not self-medication with sex, wine, or cannabis. At 35, a few weeks before a scheduled oral presentation for her Ph.D thesis in molecular biology at Duke University, she drove alone to the North Carolinia shore, shoved a bureau against her motel room door, and swallowed chloroform, more than 25 times the lethal dose. Two days later, she was discovered in a coma and sent for her first long stay at John Umstead state hospital—the place to which she was returned after she jumped from Duke Medical Center two years later.
By then, she was like a cat with nine unwanted lives: she had lost faith even in her ability to kill herself. “I had given up on pills, “ she says. “Guns are foreign to me, and I knew I couldn’t get a license even if I’d wanted one. I decided that it wouldn’t matter what I did; I would be brought back to the hospital and have to start all over again. I wanted to die, but the powers that be, the gods, were not going to let go of me.”
That fall, she was forced to take part in a psychotherapy that integrated western behaviorism with Zen, mindfulness practice, and what its developer, Marsha Linehan, a Catholic psychology professor and Zen practitioner, called wise mind and radical acceptance. Ten months later, Kandel left the hospital. In the eight years since, she has never come close to being re-hospitalized or to killing herself.
It is October 5, 2000—an overcast day in Seattle—and the Art Deco ballroom of the Edmund Meany Hotel is crammed with psychotherapy’s ground troops—social workers, psychologists and case managers from agencies and HMOs throughout California and the Pacific Northwest. On the dais stands Marsha Linehan, a psychologist and researcher at the University of Washington and an upright, energetic woman wearing a bright silk scarf over a dark dress. She holds a wooden striker in front of the bronze bowl of a Densho bell used in Zen centers to announce the start of meditation.
“We are going to work on the first mindfulness skill, which is observing,” drawls Linehan, a native of Oklahoma, in a voice equal parts authority and honey. “Usually we think of meditation as relaxation, as feeling better. But it’s not necessary to get calm, comfortable and soothed. The idea is to try to do only one thing at a time. Just notice the sound.” She strikes the bell gently, drawing out a warm velvety hum that vibrates heart and stomach from the inside. Then she rattles her wooden striker across its dimpled surface and strikes again, hard, with a clattering clang, so that people nearly jump. Wake up, wake up, the bell says. Pay attention.
The room is quiet, the therapists focused. But this is no mindfulness retreat: they’re hear to learn Linehan’s Dialectical Behavior Therapy (DBT), now widely believed to be the most effective way to treat people like Kandel, diagnosed with borderline personality disorder.
The term borderline—originally used in 1938 to describe clients supposedly “on the borderline” between psychosis and neurosis—has become a code word for clients that many therapists avoid because of the pity, anger, hopelessness and fear they can arouse in those who try to help them. Think of the people Freud called “hysterics,” like Dora and the Wolf Man; think of the alcoholic, dishonest and fragile Blanche Dubois in A Streetcar Named Desire, eternally dependent on “the kindness of strangers.” Think of Marilyn Monroe—sexually abused as a child and abandoned by her psychotic mother—forever wandering into exploitative relationships, a walking victim. Think of Alex Forrest, the seeming self-sufficient Manhattan book editor played by Glenn Close in Fatal Attraction—careening from seduction to loneliness; from wrist-slitting to stalking and vengeance. On a very bad day—when you are trying more frantically than usual to cling to what you think makes you happy and push away what you think makes you miserable—think of yourself.
Seventy-five percent of “borderlines” have a history of childhood sexual abuse, and others survived other forms of trauma. Seventy-five percent are women. Many try to kill themselves. Nine percent succeed. Psychotherapy had little to offer them until 1991, when the scientifically authoritative Archives of General Psychiatry published a study by Linehan of her federally funded work with twenty-two self-destructive Seattle women. All had tried to kill themselves at least twice and many practiced “parasuicide”: they addictively attacked their own bodies in moments of emotional crisis, slashing forearms, tendons and wrists; garroting themselves; burning themselves with cigarettes and lighters. After four months of DBT therapy that included weekly training in mindfulness and interpersonal skills, fewer than half continued to harm themselves, compared with roughly seventy-five percent of a comparison group of twenty-two treated by other Seattle therapists. By the end of the year, they had harmed themselves significantly less than the control group and spent significantly fewer days in mental hospitals.
Since then, more than 100,000 therapists have bought Linehan’s psychological texts, and tens of thousands have taken her introductory DBT training. Perhaps the most articulate advocate for borderline individuals ever to appear in the mental health field, Linehan—previously a little-known researcher—turned out to have an uncanny knack for explaining the borderline’s inner world in terms anyone could understand. Borderline individuals, she theorized in a dense, heavily footnoted 1993 text (Cognitive-Behavioral Treatment of Borderline Personality Disorder), had “no emotional skin” and were raised in families where their extreme sensitivity was routinely laughed at, criticized, or ignored. This had bred profound self-distrust, a tendency toward extremes and pervasive “emotional, behavioral, interpersonal and cognitive disregulation.”
Therapy, she wrote, repeated the pain of the invalidating family when it offered insulting interpretations, ignored cries of distress, or inadvertently rewarded tantrums or suicidality with extra attention or hospitalization. In an unconscious echo of the Buddhist notion that there is no fixed and permanent self, borderline individuals, she wrote, had huge deficits in life skills—not deficient personalities. Teaching them better ways to manage their moods and cope with the world, she theorized, would reduce their self-destructive behavior.
This could be best accomplished, she suggested, by pairing therapy with a weekly “skills training” class that blended Western assertiveness training with Eastern mindfulness. Her manual for the classes (vetted, she says, by two of her Zen teachers) includes mindfulness exercises and lengthy quotations from Thich Nhat Hanh on “washing the dishes just to wash the dishes.”
The work is scrupulously grounded in Western behaviorist psychology, but Linehan, ever an experimental scientist, continues to throw in anything that might work. On the second morning of her workshop in Seattle, for instance, her Densho bell gives way to Greek music and she makes the therapists execute the intricate steps of the hora. “Throw yourself into it!” she urges, as people sway back and forth in more or less graceful lines, practicing “one-mindfulness” and “wholeheartedness.” “Your job is to learn the skills yourself,” she says. “If you can do them, you can teach them.”
“The skills” turn out to be a bewilderingly promiscuous gumbo of attitudes, emotional techniques and psychosocial skills that seem, at first, self-contradictory: behaviorist “diary cards” and Greek dancing; radical acceptance of things as they are and assertiveness skills for changing them; “distress tolerance” and “emotion regulation” for facing fears head-on; the measured deliberation of writing out lists of pros and cons before acting. Nobody is playing with a full deck, she suggests, and skills training provides the missing cards.
Linehan sometimes jokes that she could have named her treatment “Zen Behavior Therapy,” but it wouldn’t have been a good career move. Instead, she called it Dialectical Behavior Therapy, a reference to the propositions elaborated by the ninetheenth century German philosophers Immanuel Kant, Friedreich Hegel and Karl Marx. “Dialectics” is a western description of the notion that there are two sides to every coin, and the coin cannot exist without them. Every extreme in thought and in the world calls forth its opposite and points the way to a synthesis or reconciliation. Dialectics perceives the world as an eternal dance of related opposites, like the black and white Taoist fishes chasing each other on the Ying-Yang symbol; as in the Heart Sutra, form and emptiness interpenetrate each other and make a single whole. Humorous and wide enough to cope with paradox, Dialectical Behavior Therapy—like a good Zen teacher or life itself—sometimes simply holds contradictions in balance rather than integrating them. “You’re perfect as you are—and you’ve got to change,” Linehan tells the therapists, echoing the question investigated by Soto Zen master Dogen : if all beings have Buddha nature, why do we need to practice? : (Or the koan: If the wind is always blowing, why do we use a fan?) That,” Linehan goes on, “Is the essential dialectic of the treatment.”
Marsha Linehan is fifty-eight and lives in a warmly painted bungalow walking distance from the University of Washington and the Edmund Meany Hotel. On the edge of a kitchen, a row of Post-It notes reminds her of back-to-back weekend appointments. On a living room table in the living room stands a photograph of a smiling, white-haired man in black robes—Linehan’s Zen teacher, a German Benedictine monk named Willigis Jager. She speaks of her life and its curious, seemingly random entwinement of Catholic mysticism, rigorous western science, and Zen training.
One of the six bright children of a Tulsa oil executive and his wife, she was raised as a Catholic, reading the lives of the saints and dreaming of becoming a nun. She once told an interviewer that in her early 20s, she had an experience her Zen teacher later characterized as enlightenment—an experience that changed her life. But she will not speak of that today.
In the early 1970s, she says, she continued a devout and prayerful path in college while her spiritual ambitions secularized. With a new Ph.D. from Loyola Institute in Chicago, knowing only that she wanted to work with the most miserable people in the world, she took on her first distraught and suicidal clients as an intern at a suicide-prevention clinic in Buffalo, New York. In love with psychology as a science, she wanted to pay attention to observable behaviors rather than speculate about motivations. Never willing to ascribe intents she could not verify, she theorized that cutting and suicide attempts were problem-solving attempts, not manipulations. Like a good Buddhist, she did not see the “selves” of her damaged clients as fixed, separate and eternal: she assumed that their self-punishing responses were learned, the inevitable result of certain causes and conditions. And that these responses, she theorized, could be unlearned when causes and conditions changed.
She did not speak in Buddhist terms. Even now, after ten years of Zen training, she considers herself a Catholic, not a Buddhist. But she brought to her work the precise nonjudgmental awareness cultivated by vipassana, or insight meditation, and other Buddhist practices. First she tried to get her clients to engage in a step-by-step dissection of the triggering events, thoughts and feelings that led them to the moment they tried to kill themselves. It was like trying to build a wall of pebbles in a rushing stream: when she suggested role-plays or topics that frightened them, her clients either attacked her for not caring or withdrew. When she was warm and validating, they relaxed—but continued to lead lives so filled with crises that she could not teach them the life skills they desperately needed.
Stymied, she did more research, got more training, studied to become a spiritual director in the Catholic tradition, and continued to pray and meditate alone. In 1977 she took a position at the University of Washington and there, over the next eight years, she added and subtracted therapeutic devices plundered from every conceivable source, while graduate students filmed, watched and encoded her sessions from behind one-way mirrors.
Instead of constructing a grand theory, Linehan broke down the borderline dilemma into bite-size pieces and resolved them one by one until her therapy included everything but the kitchen sink. To stop current emergencies from overwhelming attempts at change, she separated out a weekly “skills training” class. Hypothesizing that self-injury halted neurobiological cascades of unbearable feeling, she read the research on delayed gratification and asked friends how they got through difficult times.
The result was a handout on “distress tolerance”: simple tips for self-soothing and self-distraction like taking a bath, thinking of someone more miserable than you or lighting a candle and watching the flame. When a client discovered that holding a cube of ice often quelled her urge to cut herself, that, too, became part of skills training.
Because Linehan found that even her most competent-looking clients often did not know the basics of negotiating with others or acting independently of current mood, the “skills training” syllabus grew to include sections on interpersonal effectiveness and “emotion regulation”—nonjudgmentally observing current emotions, and acting despite them. Then, in 1986, when she was 42 and suffering from a dryness in her own spiritual life, Linehan picked up a Zen book at a bookstore with the word “nothing” in the title and impulsively took a year’s leave of absence to train in Zen monasteries in California and Germany. For the first time in years, this forceful, strong-willed woman followed instructions instead of giving them.
At the Anglican-influenced Shasta Abbey in northern California, founded by Jyushu Kennet Roshi, she hauled sheep manure, picked beans, sat zazen (Zen meditation) and submitted herself to bells and schedules. From this experience, she drew what she later labeled “one-mindedness,” “wholeheartedness” and “willingness,” and incorporated them into skills training. “The idea was to give up ego every way you could, to do what was called for in every moment,” she remembers, glancing at her photograph of Willigis Jager. “We would sit in the mornings and chant, and then file out and get a work assignment and try not to want a particular assignment. When they rang the bell and work was over and you were in the middle of sweeping, you had to stop in mid-stroke, because, otherwise, you were doing it for your own ego.”
Easier said than done. Linehan says she was a “high-maintenance Zen student.” After three months, she went to a priest and dramatically told him she was on the edge of spiritual breakthrough and wanted to sit nonstop for three days. The monk took her hyperbole seriously, saying he was sure she knew what she needed. But since Shasta Abbey didn’t do things that way, why didn’t she go to the nearby Holiday Inn, meditate for as long as she liked and then come back? Out on a limb not of her choosing, Linehan backtracked and returned to the schedule. She has since integrated the monk’s technique into DBT, describing it as similar to an Aikido strategy, in which an attacker’s thrust is drawn out to the tipping point where she loses her balance, called “extending.” When a suicidal new client once told her dramatically, “Either I have to do this therapy or I have to die. Those are my only two choices,” for example, Linehan asked coolly, “Well, why not die?” Taken aback, the woman replied, “If I’ve got one last hope why not take it?” and Linehan closed in, “So all things being equal, you’d rather live than die. That’s good. That’s going to be your strength. We’re going to play to that.”
Next Linehan underwent koan practice with Willigis Jager in Germany and felt, for the first time in her life completely accepted and understood. Her relationship with him is now the model for her relationship with her own clients. During one sesshin—a ten-day period of intensive Zen practice—she got a letter from her mother, who was dying. Dimly intuiting that her tears were about more than her mother, she cried in the meditation hall for three days straight, bowing, sitting and crying through her daily sanzen interviews with Jager. He would say only “Keep going,” and ring his bell to signal that the interview was over. After three days, Linehan came into the interview room no longer crying. He moved on to the next part of their koan practice without comment. “It taught me that everything is as it is, and you don’t have to change it,” she remembers. “And that has also found its way into my treatment.” She still practices with Jager almost every year.
Linehan came back to the University of Washington with a deepened ability to accept life as it is. Zen training had made her joyful and happy, and she wanted to share its benefits. “I don’t believe anyone is different. Humans are humans. We all have a physiology that’s similar, a psychology that’s similar. And if it worked for me, it will work for them. If I could learn to walk, they could learn to walk. If I could learn to be happy, they could learn to be happy. All I had to do was figure out how to teach it.” At first she tried to import Zen wholesale, trying unsuccessfully to get her clients, among them homeless women, prostitutes, drug addicts and alcoholics, to take off their shoes and walk meditatively and loosely “like water buffaloes” down the clinic halls. It didn’t translate.
Since then, Linehan has distilled a Zen completely denatured of ritual, robes or religion—epitomized in one of the two central poles around which her therapy now revolves, which she calls radical acceptance. Radical acceptance rests on letting go of the illusion of control and a willingness to notice and accept things just as they are right now, without judging—all of it, with its mistakes and messiness, pain, surprise, and impermanence.
Over time, this emotional resting-place has helped Linehan and her trainees tolerate their clients’ pain without protecting themselves with distance or blame; it has transformed their work. At staff meetings at the University of Washington, Linehan’s team now rings a second mindfulness bell to signal the need to pause and take a breath whenever anyone says anything judgmental about a client, another therapist or themselves.
All easier said than done: DBT remains a long journey for both client and therapist. Susan Kandel, for instance, was utterly skeptical when she and her fellow inmates at John Umstead state hospital were first exposed to DBT. “We hated it,” she recalls. “We had come into the hospital with our lives almost gone, and we had tried to kill ourselves in serious ways. Now we were being asked to fill out diary cards like we were in elementary school and participate in stretches in the dayroom. Give me a break!”
But that Christmas, cold and miserable, Kandel asked the staff psychologist, Meggan Moorhead, to help her get through the two-week staff vacation when activities shut down. Moorhead wrote out a list of ways Kandel could distract herself or practice mindfulness, and Kandel held on to the paper like a map out of hell.
She had long used self-harm to regulate her emotions. Now, she tried not making a bad situation worse, and followed her breath rather than thinking about cutting herself. She often took two steps forward and one step back. But Moorhead relentlessly applauded even her smallest move in the right direction, and over time, Kandel’s behavior became less mood-dependent.
With many a stumble, Kandel thus embarked on a process of attentional, behavioral and emotional training within an intimate therapeutic relationship—a relationship with echoes of the Asian teacher-student relationship as well as of traditional western psychotherapy. Together, they moved towards a sort of change better described by Soto than Rinzai notions of awakening: not the drenching thunderstorm of sudden enlightenment but the hope that after months and years of plodding across misty fields, their robes would be soaked through.
In June 1994, after agreeing not to harm herself or use alcohol for three months, Kandel was discharged from John Umstead state hospital. She continued her skills training class as and saw Meggan Moorhead for therapy as an outpatient. She went to live in the only place that would take her—a rest home full of elderly people in a desolate neighborhood of Durham. Still in chronic pain from her back injury, lonely and knowing nobody, Kandel had her first ordinary-life experience of a fundamental DBT skill that Linehan calls wise mind. “I was standing outside thinking, ‘Everything is so bad and hopeless,’ and I was starting to think my whole future was bad and hopeless,” Kandel recalls. “I remembered Meggan saying, ‘Suffer one moment at a time’ and ‘Don’t decide on the future when you’re feeling bad. Come back to this moment.’”
“So I said to myself, ‘Right now I feel really bad, and that’s all I have to think about,’ Kandel explains. “Not worry about an hour from now, let alone tomorrow. And that didn’t seem nearly as intolerable. A huge breath of relief just came out of me.”
The moment helped her shift away from the self-perpetuating cascade of thoughts and emotions that had so often led her to harm herself. “Since it was just this moment, and not the future, then I could more easily problem-solve with a distraction,” she remembers.
“You can’t distract for your entire life, but for the moment, it’s okay.” Kandel wasn’t the only one who needed radical acceptance. “I had to radically accept that this individual was in so much pain,” her therapist, Meggan Moorhead remembers. “When I had to leave for a conference, I knew Susan was going to work herself into numbness and stay frozen for seven days. I had to go anyway and accept that there was that much suffering in the world and in this individual. There were times when we were both verging on hopelessness. I had to accept that and keep trying to make a difference together.” Over weeks, months and years, she and Kandel analyzed the chains of behavior that led her to dire states or ineffective actions and brainstormed alternatives. Moorhead was the cheerleader, holding Kandel’s hand, encouraging change and yet modeling acceptance. She reframed Kandel’s behavior as the product of a “problematic learning history” rather than mental illness or innate evil; she talked to Kandel weekly on the phone, suggesting skills to try—and Kandel was almost always willing.
Using the DBT skill called participate, Kandel volunteered at a Durham hospital, taking care of babies while their mothers got counseling. She went to therapy, filled out diary cards, practiced mindfulness, walked and read. She got a job in a gift shop. Coached by Moorhead in “interpersonal effectiveness” skills, she lobbied her way back into her old halfway house in Chapel Hill, which had been terrified to readmit her for fear she’d try to kill herself. She got a better job, at a law firm. And she began going to work no matter how she felt.
“As much as I didn’t want to go, boy did I feel better by the end of the day. I’d say, ‘Boy I did it, man,’ and that was mastery,’ right there,” she says. “A lot of suicidal self-destructive stuff started to just leave me. I wasn’t putting on a façade. I was plenty scared and plenty depressed, but I was functioning, I was behaving, I was doing okay.” Out of the scraps of her life, she began the meticulous construction of a self. Like an image slowly developing in the photographic solution in the darkroom, a life began to emerge dedicated to something other than escape, withdrawal and self-injury.
Developing a Self
Using a therapy heavily influenced by Buddhism, which theorizes that the notion of a fixed, independent and permanent “self” is a convenient fiction, Kandel began to develop a self. She could pause, make choices, and shift her attentional state, to respond rather than react. At first, she used “the skills” like someone driving while referring to a map; later she developed an inner compass. Once she had seen herself as fundamentally evil and incapable of change—a bad seed, a lunatic. Emotion had regularly driven her into the mouth of hell, without a sense of choice or freedom. Now, she learned to pause and observe and describe her experience, noticing the evanescence of emotions that she neither resisted in panic nor invited in for tea. She discovered a love of horticulture and took classes at the local community college. She found a job in a plant nursery. She is now much more closely connected to others, less isolated and yet more capable of self-care, and in a strange way, more self-reliant.
“I’ve learned the skills, the symptoms have eased and there’s been a major structural change,” she says now, looking back. “I see my character very differently. I don’t see my structure as weak or fragile. Vulnerable, yes, but I don’t think vulnerability is a bad thing. I used to think that the world was essentially bad, and I don’t see that anymore. When I look at the world now, I see the good. I see the connectedness between all of us, and I don’t see the alienation, the disonnection. We’re all in this together.
“DBT is mundane, like physical therapy for a person who’s broken her leg in fifteen places and been told she’ll never run again,” she goes on.. “You do it step by step; it hurts, it’s boring. Something changes, but there isn’t a single dramatic moment when you throw away your cane.” A Box with 100 Things in It
Meanwhile, Linehan herself doesn’t know exactly where the magic and the limitations lie. “It’s like finding a box with 100 things in it and not knowing which three are really that good,” she says. “It could also be that it just energizes therapists and give them hope.” As a scientist intimately familiar with Zen notions of nonattachment, she remains more wedded to truth and experiment than to pet ideas. “My greatest fear,” she wrote in a successful application for senior-scientist grant from the National Institute of Mental Health, “is that therapists and patients doing DBT will become attached to the therapy itself rather than to empirical effectiveness.”
Among the most compelling results so far are those of the Greater Manchester community mental health agency in southern New Hampshire. In 1994, after instituting DBT, combined mental and medical treatment costs for their fourteen most expensive and self-destructive borderline clients fell by fifty-eight percent—from a total of $645,000 to $273,000. The agency gave the clients more therapy, but the cost was more than offset by a seventy-seven percent decrease in hospitalization days, a seventy-six percent decrease in day treatment and an eighty percent decline in 911 calls. Only two of the clients were employed when treatment began; eight had jobs at the close of the first year.
“DBT has given us hope that was not there seven years ago,” says counselor Patricia Carty of the agency, which has since implemented DBT system-wide. “We now have confidence that this population can be effectively treated and we can see people recover from this disorder.”
A Life Worth Living
Susan Kandel no longer spends days stewing in depression or cuts herself. She speaks of The Skills in capital letters, the way one might quote a sacred text. It has been eight years since she sat in a state mental hospital grasping a piece of paper that described how to “not make a bad time worse.” She can eat when she’s hungry, take a shower when she aches, mend a shirt or walk in the woods when discouraged, notice and enjoy the smell of spring leaves and feel the sun against her skin. Badly shaken by the World Trade Center bombings, she began, in its aftermath, to practice the Tibetan meditation popularized by Pema Chodren and known astonglen, first on her own behalf, and then on behalf of others. While a friend—a therapist and spiritual teacher—volunteered as a counselor in Manhattan, Susan was in Chapel Hill doing tonglen on her behalf—breathing in the woman’s fear, and breathing out self-compassion and non-self-judgement for her.
Kandel’s transformation is the result of a normal accretion of small changes, a journey not peculiar to “borderlines” but familiar to anyone who has tried to stop biting her lip or become more assertive, less reactive or more kind. “There’s no magic to it,” Kandel says, looking back. “It’s not like being born again through your mother’s womb. It’s based on things people take for granted—things you can find in the dictionary.” Thus, she has been brought back within the circle of normal human behavior with the rest of us, where she always belonged. Nobody would confuse her now with a fictional character from Fatal Attraction or A Streetcar Named Desire and she no longer meets the criteria for a psychiatric diagnosis of Borderline Personality Disorder. As she puts it, “I don’t do borderline any more.” ▼
Thank you for subscribing to Tricycle! As a nonprofit, we depend on readers like you to keep Buddhist teachings and practices widely available.