Bringing a Buddhist view to the care of the dying was the subject of five recent interviews conducted by Mary Talbot, Executive Editor of Tricycle, and combined into the following discussion.
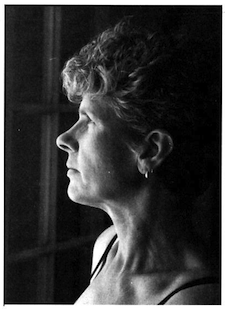
Joan Halifax, a medical anthropologist and author, began her work with dying people in 1970 at the Miami School of Medicine. She is a senior teacher in Thich Nhat Hanh’s Order of Interbeing, founder of the Ojai Foundation, Upaya, and The Project On Being With Dying, and a founding teacher of the Zen Peacemaker Order.
Christine Longaker, is a cofounder of the Hospice of Santa Cruz County, the founder of Rigpa Fellowship in the United States, and the author of Facing Death and Finding Hope: A Guide to the Emotional and Spiritual Care of the Dying (Doubleday, 1997). For twenty years she has taught courses on the contemplative care of the dying.
Barbara Rhodes is a registered nurse and coabbott of the Kwan Um School of Zen in Cumberland, Rhode Island. She works for Hospice Care of Rhode Island and has ministered to the dying for more than twenty years.
Jeanne Anselmo, a student of Thich Nhat Hanh, is a holistic nurse in New York City. She has worked with the dying since 1974.
Kathleen O’Rourke studied with Maezumi Roshi and works with The Project On Being With Dying in Santa Fe, New Mexico.
TRICYCLE: Joan Halifax, how did you come to work with the dying?
HALIFAX: My grandmother from Savannah, Georgia, with whom I spent a lot of time as a child, took care of many of her friends when they were dying. After they died, she dressed them and saw the family through their grief. It was part of the life of a Southern woman to do that. Being with the dying is the work of village women everywhere. The fact that my grandmother was comfort able with dying people and dead bodies undoubtedly influenced why I grew up without much fear of death.
TRICYCLE: And eventually you came to work with the dying in a professional setting?
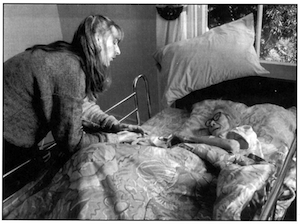
HALIFAX: Yes. In 1970 I went to work at the University of Miami School of Medicine as a medical anthropologist. Dying people were basically ignored in hospital settings because they were a “lost cause.” In 1972, I married [psychiatrist and LSD researcher] Stanislav Grof, and we worked with people dying of cancer, using LSD as an adjunct to psychotherapy. I was inspired to be with people who were facing extreme situations. During the LSD sessions, I was usually lying on the couch with the dying person, holding him or her. Often I felt like a mother who was holding her suffering child or a child holding a dying parent.
TRICYCLE: Jeanne Anselmo, is palliative care of the dying part of a nurse’s training?
ANSELMO: Not in 1974, when I began working at Sloan-Kettering, and only now are we beginning to try to change that. As a student, there were times that I’d know one of my clients was dying, even if I was at home. I just had a sense about connecting with people in some way, talking to them—nobody had even mentioned that in the training. I was learning about what it was like to be with a person who was dying, that each death had a different energy and tempo and rhythm, and that it had nothing to do with what the doctors talked about in terms of prognosis. The people we were told would soon be released from the hospital often went into their own dying process, and died. And often ones who we were sure were going to go-they lived very long and healthy lives.
TRICYCLE: Christine Longaker, your husband’s death led you to the hospice movement?
LONGAKER: Yes, twenty-one years ago my husband was diagnosed with acute leukemia. It was really my first personal encounter with a death, and I realized I didn’t have a clue what death was. I didn’t have any spiritual belief at the time, or any images or concepts about death. All I could draw on was what I had learned in our society, which is that it is some thing very tragic and hopeless. And I said to my husband, “If that’s all that death is, then we’re just going to feel like victims of this illness and the rest of the time that you live, our lives will just be a sad story playing itself out.” So we decided instead to view death as a gift in our lives. This view of death helped us get through the suffering of that year and find a deeper appreciation of life. By the time he died a year later, when we said our goodbyes, we had a feeling of “Thank you. I’m sorry for all the trouble that there’s been, but at the same time, thank you for being there, and for this year, and for what we’ve learned together.” And that allowed me to feel very peaceful at his death.
A year later, I joined a group of people in northern California who were starting a hospice program. Because of the positive aspects of my husband’s death, I had a strong wish to give something back to others. I hoped I might help other people avoid some of the unnecessary suffering my husband and I went through during the year of his illness.
TRICYCLE: What can you offer to someone who is dying?
HALIFAX: Most of what we are “doing” is listening. Usually, we’re not doing guided visualizations. We’re not giving advice. We’re not doing psychotherapy. We’re not administering medications. We are being present. And that presence requires listening—to what is said, what isn’t said, even to silence. One person I worked with, a very wonderful man, had just gotten discharged from the hospital and he said, “Thirty, forty, fifty people come see me in a typical hospital day, asking me questions. Not one person sat in silence with me, and that’s all I wanted. Just somebody to be with me.” That’s our true work. It’s not applying fancy meditative technologies. It’s practicing radical optimism. In this work, you need to be fearless. And that’s what we give: no fear.
TRICYCLE: Barbara Rhodes, is “no fear” a state you bring to your work?
RHODES: I just try to be myself, which is usually pretty fearless, and I think that provides some comfort to people. I work with respecting them and making a lot of eye contact and trying to remind them of their qualities and strengths and really encourage them to find out who they are before they go. I think that helps fear go away. Of course, believing in themselves is work that they have to do on their own. But I think seeing and paying attention to them helps someone who’s dying feel a little more solid. They often need less [pain and anxiety] medication as a result.
TRICYCLE: Determining what someone needs must be a very subtle process.
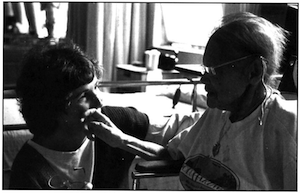
ANSELMO: Often I find that when people are dying, there’s a way in which we start to connect, there is an energy beyond conscious mind that starts to unfold. That is what teaches us what we need to say or pay attention to. There are so many ways to help to reassure a person. I try to really pay attention to who that person is. As a nurse, I maybe just sit, or just breathe with the person, or use therapeutic touch. Or I mayencourage friends and family to come in. Basically, I’m trying to read what the person is saying on so many subtle levels of their being, whether it’s in the intonation of their voice, their nuances, or their breathing pattern. Sometimes that’s all you need to hear.
TRICYCLE: Kathleen O’Rourke, when you were diagnosed with breast cancer two years ago, did you imagine that you would be helping other people to die?
O’ROURKE: Well, that diagnosis was my first real hit that I might die soon. At the end of my treatment, a very close friend of mine got sick with lymphoma. She did everything she could, all the treatments that she could, and it just wasn’t working. She became bedridden and needed round-the-clock help. We needed a schedule for her, and Joan [Halifax] helped us with that.
Since then, I have sat with others through Joan’s Partners Program, where we sit with someone who is dying. There’s something about what I’ve done and the experiences I’ve been though that’s very attractive to people who find themselves in the midst of cancer or whatever it is.
TRICYCLE: Christine, you use the term “unconditional acceptance” of the dying. What do you mean?
LONGAKER: I remember years ago hearing Elisabeth Kubler-Ross say that the dying need unconditional love. I really took that to heart and realized that I hadn’t experienced that toward my closest friends, let alone myself. I imagine it is a state pretty close to enlightenment. So I wondered, what could I give the dying—or the living for that matter—that comes close to that? And what I came up with was unconditional acceptance. We need to accept them exactly as they are, understanding that they are human beings with suffering, with habits, with a whole history we might not understand.
TRICYCLE: Can you separate physical from spiritual care?
HALIFAX: Definitely not. Often people are not only physically neglected but physically traumatized in the process of illness. To be touched or held can be so beneficial, whether it’s the therapeutic touch of a nurse or the touch of the doctor on your hand, or of a relative or a friend just holding you. Neglect often comes out of fear of being in contact with a dying person.
TRICYCLE: Is it ever hard for you to be in the presence of that kind of suffering?

HALIFAX: Being in the presence of suffering, we can experience alienation and defensiveness, or dualism can dissolve and compassion arises. If you feel alienated, then you know you are protecting yourself. It’s very common to objectify sick people, to classify them as a “cancer patient” or as a “colostomy.” We try to “deobjectify” people, to realize the truth of non-differentiation between self and other. If you are able to be fully with someone, you see that the illness is yours. The work focuses on developing compassion and equanimity, the two sides of the coin of non-dual awareness. We try to exemplify the internal qualities that we hope will develop in the dying person, where he or she can be present and sustaining in the face of great physical and psychological difficulties.
TRICYCLE: What does Buddhism have to offer non-Buddhists who are dying?
RHODES: The Four Noble Truths are grounded in the fact of suffering. People might think that’s negative, but it’s only the truth. It’s our human condition. So Buddhism has us just look at it nakedly. Look and ask yourself, “What is this? What am I?” That’s the last thing a lot of people want to do, especially when they are sick. They want to be fluffed up somehow, diverted. But Buddhism doesn’t allow that, and hospice doesn’t allow that.
HALIFAX: Death has been a very important teacher for Buddhists through the centuries, and I think that’s why Buddhism has so much to offer to our understanding of death and dying today. It all starts with the Four Noble Truths on suffering and freedom from suffering. Then there are all the contemplative technologies, from meditation to phowa. It’s been said by many teachers that there are only two kinds of meditations we need to practice, one is lovingkindness and the other is the awareness of death. I think that is very good advice. But most important, Buddhism’s perspective on liberation at the moment of death lies at the heart of our work. Death is the most radical opportunity for enlightenment.
TRICYCLE: And the teachings on impermanence?
HALIFAX: I remember one man with AIDS I worked with in Georgia. He came into a retreat for dying people and caregivers. In the retreat, I talked about impermanence and we did some practices focusing on impermanence. In the final phase of his illness he said, “You know, I’m so glad you told me about anitya [impermanence]” like it was a woman. “Anitya really helped me. If I thought I had to live with this pain into eternity, I would go mad. But knowing that this pain is impermanent, I can be with it, finally.”
TRICYCLE: Christine, coming from a Tibetan tradition, do you automatically bring the teachings on the bardos and rebirth to bear in a hospice setting?
LONGAKER: When I was doing caregiving work, I found the teachings on the bardos heightened my awareness of, and understanding for, the deep suffering the dying person was experiencing. I didn’t speak to them about my beliefs—it wouldn’t be appropriate in that type of setting.
But the Tibetan Buddhist teachings say that those who care for the dying can give invaluable support if their meditation practice has stabilized to the point where they rest continually in their true nature of mind. My meditation practice is not that advanced, so I rely on the “essential phowa” practice that I learned from Sogyal Rinpoche. It can be used to heal the regrets and the memories of our life. It’s a practice for life and it’s also the main practice we rely on after someone has died, to help free them of the suffering.
TRICYCLE: Joan, do you bring up Buddhist practices or ideas or terms with people who have no familiarity with the teachings?
HALIFAX: Only when it’s appropriate, though I do get asked about it by people who know I am a Buddhist. Our Partners Program, for example, is made up mostly of so-called non-Buddhists. They have learned that we are not helping Buddhists to die, we are helping buddhas to die. That’s a major distinction. We work with Christians and Jews and agnostics, so we have to translate Buddhism for a population which is not Buddhist.
RHODES: I don’t. In eleven years, no one has ever asked me for a book or a specific practice to do. Rhode Island is a very Catholic state, and those who don’t have some established religion are agnostic. My teacher says, “An old man can’t practice.” And that’s not about putting down seniors. It’s about an encrusted consciousness that can’t change. And I think when you are dying, you’re even less likely to make a shift. Some people think that dying is an opportunity to open, but I haven’t seen that. In my experience it’s more likely to push you into your habits and fearfulness more.
TRICYCLE: But you challenge that encrustedness? You try to move the person away from their habits?
RHODES: I’ll test the waters and say, “Would you like to sit with me quietly for a while?” And some people like that. And sometimes I think maybe I should try more.
TRICYCLE: Do you have specific techniques or practices you use in trying to allay someone’s fear, or to help them tap into their true nature?

O’ROURKE: I think it’s a very individual thing. My Zen practice has taught me a great deal, but a lot of what I do I learned in A.A., which I’ve been in for fifteen years. I often ask people if there is a place internally where they can feel comfortable. And most people say, “Yes.” And then I ask, “How can you access that? What are the things you do?” And mostly, I think, it’s a quietness, a conscious touching of that place. I think the same thing happens with the metta practice that Joan does, but without the directions.
RHODES: After I know a patient well enough, I take the risk of asking them about certain things: What’s the point? And what was most important about your life? Or if there is something afterward, what do you think it might be or what would you like it to be? I try to get them to start thinking, and if it makes them really uncomfortable, I stop.
I took a workshop with Patricia Shelton [guiding teacher of the Clear Light Society] on the breath meditation practice she does with the dying, where you say part of a prayer or chant on the patient’s exhale [see p. 64]. The first time I used it was with a family—sort of your average Catholic family—whose father was dying from cancer. I suggested we try this meditation, saying a phrase of the Lord’s Prayer on his exhale. Some of them kept going out of the room because they couldn’t handle the intimacy, which was very intense. Just to be able to say, “Our Father…”—he was breathing slightly —”…who art in heaven….” It was beautiful. We did it for about forty-five minutes without stopping, and it was like being at a Zen retreat.
The family really responded and relaxed and, you know, there was no patient there, we were all dying. And after having a really pained expression on his face, the man relaxed. He died with a smile on his face. It was incredible.
TRICYCLE: Do you try to figure out if someone has a spiritual base and tap into it?
RHODES: In my experience, I often need to bring it up, I need to search that out a little bit. I’ve had some very evolved patients who teach me as much as I could possibly teach them, who are very open and honest about their process. But still most of them, I think, are pretty fearful. Even though they are open and honest and good communicators, there’s an edge where they feel tight and afraid, and I think that’s my experience: there aren’t too many people who are prepared to die, are prepared to relax and trust it, sit in the corner and just not know and be with it, learn from it.
TRICYCLE: Christine?
LONGAKER: I once worked with a woman with advanced cancer who noticed how at ease I felt about death. She kept asking me, “What do you know? Why are you so confident about facing dying and death with me?” She told me, “l study with the Church of Religious Science, and we are open to every religious tradition, and we give teachings from every religious tradition and I want to hear what you are learning.” So I did share some of what I was learning. One of her greatest sufferings, she told me, was that her whole life she felt a strong devotion to Christ and prayed to Him and always relied on Him in times of trouble. “Now that I’m dying;’ she said, “I have so much physical suffering and so many problems in my family. And when I pray, I feel completely alone, I feel like Christ has abandoned me. “So I taught her the essential phowa practice and encouraged her to visualize and invoke the presence of Christ as she did it and to open her heart to Him and to ask for His compassion and His love and His purification. I came to see her the next week, and she said, “Before, I felt alone and isolated and abandoned by Christ. But since I’ve been doing this meditation, I feel like He’s right here in the room with me. Now I’m not afraid of dying.”
TRICYCLE: It sort of jump-started her own practice?
LONGAKER: Yes, exactly. It connected her to her devotion, but gave her a way to really bring that presence that she was longing for after death into her experience, even in the process of dying.
Even if the dying person isn’t open to such a practice, I always practice quietly by their side when I am visiting them, or when I go home at night, I imagine all the people I have met that day and I do this practice for them again and again, both when they are dying and when I’ve learned that they have died.
TRICYCLE: What do you do if someone has no spiritual path at all and is consumed with fear and anxiety?
LONGAKER: Fear and anxiety can come even for those on a spiritual path. Wherever we can, we should relieve the dying person’s fears, for example, by giving him or her adequate pain medication. Fear often comes from not feeling safe, not feeling accepted or loved, not being connected genuinely to anyone or anything. Even for someone with no spiritual beliefs, the bottom line, as the teachings say, is to help the person not die empty-handed.
TRICYCLE: Not die empty-handed?
LONGAKER: Help them find a meaning in the life they have lived. To focus on their accomplishments, on what they’ve learned, on what benefit they got from their life, on what sacrifices they made. As a friend of someone dying, you can describe to them how they have contributed to you r life, or how even in their dying, you are receiving something from them. These are all spiritual approaches, supporting someone to prepare for death from their heart and mind. There’s always something you can do.
TRICYCLE: How do you work with someone who is likely to die very soon and just doesn’t want to admit it to himself or herself?
HALIFAX: Our job is not to challenge the defense of denial, but to be present for it. Denial is an adaptation to a catastrophic situation. One woman with whom we worked had breast cancer. She was a scientifically minded woman who sought one intervention after another. Just a few days before she died, a special serum was sent from Japan by her father, who was a physician. Her husband called me up in total desperation and said, “This is insane. Two years we’ve been going through this, and she was just beginning to accept her death and now it’s another intervention and I just want to scream. I’ve been taking care of her twenty-four hours a day and I’m going crazy.” And I said to him, “If she wants it, your only job is to say ‘Yes.’ Her efforts to prolong her life are her choice.”
TRICYCLE: When someone is dying, and their emotional state is one of extreme fury or hatred, how do you handle that?
LONGAKER: If it’s someone in my family, I’m likely going to take their anger seriously at first. There’s a practice that helps me a lot: I imagine changing places with the angry person, having their suffering and seeing the world with their history of pain and fear. My compassion opens out, because I understand them, and see that they are just like me. I remind myself that their emotions and fears are only a temporary layer, like clouds moving across the sky.
TRICYCLE: What are some of the institutional or societal hurdles to doing this work?
RHODES: Sometimes the hardest thing in home care is just getting people to turn the TV off.
HALIFAX: There’s resistance in many hospital settings to pastoral or spiritual care of dying people. Those who give spiritual care are not seen as adding to the bottom line, or they’re seen as doing “light” work, whereas the “real work” is the medical stuff. Often we are not given much support. What conventional healthcare institutions often fail to realize is that spiritual care can reduce fear, stress, medications, expensive interventions, lawsuits, and the time doctors and nurses have to spend reassuring people.
TRICYCLE: Along with the fear of death and illness, is there a fear of caregivers and the care itself?
RHODES: Many people think hospice is a death sentence. Doctors don’t admit the patients to the hospice program until the very end. And that’s sad. Most patients are trying chemotherapy and radiation as long as they can. Hospice is not a death sentence. It doesn’t have to be “this means the treatments aren’t working.” But in many cases, they will die, and if they don’t come to us until five or six weeks before they die, that’s really not much time. It would be nicer to have more time with them to get to know them better and to make them more comfortable. We are very good with the medications, too, with psychosocial support and symptom control. People feel better and they are able to relax more.
ANSELMO: That affects the caregivers, too. Often people go into this experience of only being with dying, and being only with the grief and the loss and the tragedies that are occurring. It’s very difficult for people to truly replenish. And we’ve systematized it that way. We have extraordinarily gifted practitioners, but we also lose them, because they dive in so deeply.
TRICYCLE: You’ve all talked about the difficulties of walking into complex family dynamics around a death. What do caregivers need to know about that?
HALIFAX: Don’t take anything personally.
O’ROURKE: When I worked with Kathy, a woman with breast cancer, it became pretty clear that her family didn’t want me around. I was seen as a “survivor.” I picked up on it right before it happened, and I said, “I don’t think I need to be here.” I was grateful it happened, though, because I want to have my eyes open about this work.
TRICYCLE: What else has being with dying people taught you?
RHODES: It’s helped me be much more patient, with myself and others. I work full-time in hospice and I do on-call work. So I see suffering, the basic premise of Buddhism, constantly, all day long. I see all kinds of confusion and pettiness and physical discomfort and it constantly re-reminds me to practice. That’s the human condition.
ANSELMO: It has taught me to be very humble. That’s the truth.
HALIFAX: Being with a dying person is like standing in front of a mirror. You’re not looking at your own image narcissistically, you’re looking at the reality of your mortality. And it produces, frequently, the opposite of narcissism: a profound appreciation for the mystery of life and death.
TRICYCLE: Despite all the difficulties, all the cultural barriers to “conscious dying,” are you optimistic about the future of this work? For yourselves and for the culture at large?
 HALIFAX: Absolutely. In fact, I think the professionalization of this work is a problem. This is the kind of work we all should do. We should do it in our families, in our neighborhoods, in our towns. Being with a dying person is a profound privilege. The learning process is demanding and honest, and yet the skills required to do it are human and simple.
HALIFAX: Absolutely. In fact, I think the professionalization of this work is a problem. This is the kind of work we all should do. We should do it in our families, in our neighborhoods, in our towns. Being with a dying person is a profound privilege. The learning process is demanding and honest, and yet the skills required to do it are human and simple.
RHODES: People used to say to me, “How do you work in a nursing home?” And I used to say, “How can you drive by one and not go in and sit with somebody for a while?” I try not to drop my judgment, but—I love geriatrics. The people there need you so much. To me it’s the opposite of depressing. To see someone released is a beautiful thing. I’ve seen hundreds of people die, and since I’m an on-call nurse, I’m out in the middle of the night a lot. People think that I just do it because I need the money, but I do it because it is my training in Zen. And to watch someone take that last expiration and feel that silence afterward is incredible for me. That silence is an incredible teaching. It keeps my “don’t-know” mind going.
Thank you for subscribing to Tricycle! As a nonprofit, we depend on readers like you to keep Buddhist teachings and practices widely available.